About Clinical Lipidology
Over
the past twenty years international advances in the diagnosis, treatment and
prevention of artery disease have led to the development of a new specialty:
Lipidology. This new specialty is re-directing diagnosis and treatment of
artery disease, the cause of the number one and number three killers of adults:
heart attack and stroke. The American
Board of Clinical Lipidology certifies physicians in lipidology after
extensive training and a rigorous exam. There are about 700 Board Certified lipidologists in the US and Canada, but only about 50 "dedicated" lipidologists, who work exclusively with cholesterol and atherosclerosis. Regrettably, most practitioners still work with 1994 approaches, while 20 years of research have been largely ignored. But we're in the post statin age, and the number one cause of mortality (artery disease) demands state of the art care.
Lipidologists study lipids - the cholesterol and triglyceride fats that cause vascular disease and can lead to heart attack and stroke. Research has also shown the connection between lipids, diabetes, and blood pressure elevation.
International research and clinical results have shown new directions for optimal, rather than conventional, care. Lipidologists recognize that the familiar lab tests for LDL (“bad”) and HDL (“good”) cholesterol are only a starting point for understanding who is at risk for cholesterol-related disease. Lipidologists focus on treating the whole patient, not the cholesterol number. They use advanced diagnostic tests to understand who is at risk, what kind of treatment would be most effective, and to track the progress of treatment.
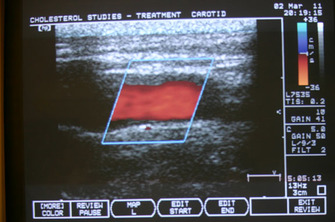
The familiar cholesterol number measures the amount of cholesterol flowing through your bloodstream. Cholesterol is an important building block of the body, and it only causes problems when it moves from the bloodstream into the artery wall, creating plaque. Lipidologists use advanced lab tests to determine whether a patient’s cholesterol is in a form likely to penetrate the arteries. They use ultrasound of the carotid arteries to visualize whether or not cholesterol is accumulating in the arteries. When plaque is present, advanced lab tests can suggest whether it is relatively stable, and less threatening, or unstable, and in danger of rupturing and causing heart attack or stroke.
Lipidologists treat artery disease with a range of natural supplements, diet and lifestyle changes, and prescription statins when necessary.
Here are some guiding principles and findings from the latest research in the field of lipidology:
1) Lowering LDL-cholesterol is not the most important target of treatment. Lowering LDL particle count--the number of LDL particles needed to transport LDL cholesterol in the blood flow-- is more crucial
2) Optimal care requires non-prescription treatments (natural supplements).
3) Circulating cholesterol comes from 3 sources. Statins primarily address only one of these sources, overproduction
4) 70% of heart attacks are caused by relatively small, non-obstructing accumulations of cholesterol that a stress test will not detect. Carotid artery ultrasound is a better indicator of the presence of these small plaques. State of the art treatment prevents, minimizes, and stabilizes these oft-ignored plaques
Here are some comparisons between the practice of clinical lipidology and standard care:
1) Clinical lipidologists are disease-based, using ultrasound visualization of arteries to determine the presence, extent, and threat of cholesterol disease, whereas standard care focuses on treating a laboratory test (LDL cholesterol)
2) Clinical lipidologists are pro-active, and use advanced lab testing to ascertain all the causes for cholesterol penetration, and work to arrest and reduce cholesterol accumulation, whereas standard care is reactive, responding when a heart attack or stroke event occurs, or when abnormal lab tests are found.
3) Clinical lipidologists are nearly 100% successful in arresting and reversing cholesterol buildup in the arteries.
4) Clinical lipidologists use multiple natural treatments whereas standard care utilizes prescription statins as the mainstay.
5) Clinical lipidologists incorporate new research in an organic, ever-changing approach to disease whereas standard care has changed little from the mid-1990’s.
Conventional care assesses your LDL-cholesterol, guesses about the degree of cholesterol penetration into your artery walls, and prescribes statins to lower LDL-cholesterol if it is elevated.
Optimal state of the art care, advanced by cholesterol specialists, assesses the presence, extent, and threat of disease in your arteries, using economic, non-radiation ultrasound. Optimal care looks beyond your LDL-cholesterol with advanced lab tests to ascertain all the causes of cholesterol accumulation in the artery wall. Optimal care starts with non-prescription approaches (supplements, dietary shifts) and uses prescriptions if necessary. Optimal care reassesses the patient after initial treatment to gauge the stabilization or reduction of cholesterol in the artery wall, evaluate the success of treatment, and modify treatment if necessary.
Who Sees a Cholesterol Specialist?
Patients with risk factors of elevated blood pressure, diabetes, a history of smoking, family members with artery disease (including heart attack or stroke), or associated diseases like rheumatoid arthritis, psoriasis, and lupus—they all benefit from an evaluation and suggestions for optimal care rather than standard care.
Patients who wonder if they really require lifelong prescription medicine for an abnormal cholesterol level are often pleasantly surprised that our evaluation shows that optimal care requires only natural treatments.
For example, here are two case histories from our practice:
Martha H., 73 years old, sedentary lifestyle, but healthy. Her doctor advised prescription Lipitor for an LDL-Cholesterol (“bad” cholesterol) of 121. Our exam revealed healthy arteries (like those we would expect to find in a much younger woman) and showed she only needed natural treatments.
Josh S., 47 years old, runs three times per week and has an excellent diet, also with an LDL-Cholesterol of 121. He is concerned because of a history of heart attack and stroke among his grandparents. Our exam revealed cholesterol accumulation in his neck arteries, with further lab tests confirming an inherited cause. He needed a prescription statin.
Cholesterol Studies and Treatment is located at 4 Calle Medico, Suite C, Santa Fe, 87505. Call 505-699-1172, or email Dr. Mickle at [email protected]
Lipidologists study lipids - the cholesterol and triglyceride fats that cause vascular disease and can lead to heart attack and stroke. Research has also shown the connection between lipids, diabetes, and blood pressure elevation.
International research and clinical results have shown new directions for optimal, rather than conventional, care. Lipidologists recognize that the familiar lab tests for LDL (“bad”) and HDL (“good”) cholesterol are only a starting point for understanding who is at risk for cholesterol-related disease. Lipidologists focus on treating the whole patient, not the cholesterol number. They use advanced diagnostic tests to understand who is at risk, what kind of treatment would be most effective, and to track the progress of treatment.
The familiar cholesterol number measures the amount of cholesterol flowing through your bloodstream. Cholesterol is an important building block of the body, and it only causes problems when it moves from the bloodstream into the artery wall, creating plaque. Lipidologists use advanced lab tests to determine whether a patient’s cholesterol is in a form likely to penetrate the arteries. They use ultrasound of the carotid arteries to visualize whether or not cholesterol is accumulating in the arteries. When plaque is present, advanced lab tests can suggest whether it is relatively stable, and less threatening, or unstable, and in danger of rupturing and causing heart attack or stroke.
Lipidologists treat artery disease with a range of natural supplements, diet and lifestyle changes, and prescription statins when necessary.
Here are some guiding principles and findings from the latest research in the field of lipidology:
1) Lowering LDL-cholesterol is not the most important target of treatment. Lowering LDL particle count--the number of LDL particles needed to transport LDL cholesterol in the blood flow-- is more crucial
2) Optimal care requires non-prescription treatments (natural supplements).
3) Circulating cholesterol comes from 3 sources. Statins primarily address only one of these sources, overproduction
4) 70% of heart attacks are caused by relatively small, non-obstructing accumulations of cholesterol that a stress test will not detect. Carotid artery ultrasound is a better indicator of the presence of these small plaques. State of the art treatment prevents, minimizes, and stabilizes these oft-ignored plaques
Here are some comparisons between the practice of clinical lipidology and standard care:
1) Clinical lipidologists are disease-based, using ultrasound visualization of arteries to determine the presence, extent, and threat of cholesterol disease, whereas standard care focuses on treating a laboratory test (LDL cholesterol)
2) Clinical lipidologists are pro-active, and use advanced lab testing to ascertain all the causes for cholesterol penetration, and work to arrest and reduce cholesterol accumulation, whereas standard care is reactive, responding when a heart attack or stroke event occurs, or when abnormal lab tests are found.
3) Clinical lipidologists are nearly 100% successful in arresting and reversing cholesterol buildup in the arteries.
4) Clinical lipidologists use multiple natural treatments whereas standard care utilizes prescription statins as the mainstay.
5) Clinical lipidologists incorporate new research in an organic, ever-changing approach to disease whereas standard care has changed little from the mid-1990’s.
Conventional care assesses your LDL-cholesterol, guesses about the degree of cholesterol penetration into your artery walls, and prescribes statins to lower LDL-cholesterol if it is elevated.
Optimal state of the art care, advanced by cholesterol specialists, assesses the presence, extent, and threat of disease in your arteries, using economic, non-radiation ultrasound. Optimal care looks beyond your LDL-cholesterol with advanced lab tests to ascertain all the causes of cholesterol accumulation in the artery wall. Optimal care starts with non-prescription approaches (supplements, dietary shifts) and uses prescriptions if necessary. Optimal care reassesses the patient after initial treatment to gauge the stabilization or reduction of cholesterol in the artery wall, evaluate the success of treatment, and modify treatment if necessary.
Who Sees a Cholesterol Specialist?
Patients with risk factors of elevated blood pressure, diabetes, a history of smoking, family members with artery disease (including heart attack or stroke), or associated diseases like rheumatoid arthritis, psoriasis, and lupus—they all benefit from an evaluation and suggestions for optimal care rather than standard care.
Patients who wonder if they really require lifelong prescription medicine for an abnormal cholesterol level are often pleasantly surprised that our evaluation shows that optimal care requires only natural treatments.
For example, here are two case histories from our practice:
Martha H., 73 years old, sedentary lifestyle, but healthy. Her doctor advised prescription Lipitor for an LDL-Cholesterol (“bad” cholesterol) of 121. Our exam revealed healthy arteries (like those we would expect to find in a much younger woman) and showed she only needed natural treatments.
Josh S., 47 years old, runs three times per week and has an excellent diet, also with an LDL-Cholesterol of 121. He is concerned because of a history of heart attack and stroke among his grandparents. Our exam revealed cholesterol accumulation in his neck arteries, with further lab tests confirming an inherited cause. He needed a prescription statin.
Cholesterol Studies and Treatment is located at 4 Calle Medico, Suite C, Santa Fe, 87505. Call 505-699-1172, or email Dr. Mickle at [email protected]
